“The daunting truth about organ failure is that it occurs in about 50 percent of all organ transplants. To help prevent rejection, transplant recipients must take highly-evolved immunosuppressive drugs, also known as anti-rejection drugs, for the rest of their lives to ensure their new organ is accepted by their body.”
Read more, here.
How a wearable helps improve care after a kidney transplant
“The wearable geko device, manufactured by UK-based Sky Medical Technology and distributed in Canada by Trudell Healthcare Solutions, is a small muscle pump activator that significantly increases blood flow via painless electrical pulses. Patients using the device following kidney transplantation experienced shorter hospital stays and reduced surgical site infections by nearly 60%.
Kidney and simultaneous pancreas-kidney transplantations can significantly reduce mortality and improve the quality of life for patients with end stage renal disease.”
Read more, here.
Despite COVID Vaccinations, Caution Still Crucial for Transplant Recipients
“Long before COVID-19 changed the world, organ transplant recipients were wearing masks to shield themselves from airborne threats.
Immunosuppressive medicines, which often are a lifelong requirement after a transplant, add an extra layer of protection against viruses as common as a cold or as dangerous as COVID. Transplant patients are told to use masks for any group gatherings or airplane flights, and hand sanitizing is a must.
While COVID has brought a heightened awareness of these patients’ health risks and fragility, a recent study by Johns Hopkins University researchers in Baltimore, Maryland, and a report from the Mayo Clinic in Jacksonville, Florida, may raise their sense of unease even further.”
Read the full article, here.
Antibody Response to 2-Dose SARS-CoV-2 mRNA Vaccine Series in Solid Organ Transplant Recipients
“Transplant recipients without prior polymerase chain reaction–confirmed COVID-19 were recruited from across the US to participate in this prospective cohort through a digital campaign. Those who completed the 2-dose SARS-CoV-2 mRNA vaccine series between December 16, 2020, and March 13, 2021, were included and followed up through April 13, 2021. As described previously,3 semiquantitative antispike serologic testing was undertaken with the Roche Elecsys anti–SARS-CoV-2 S enzyme immunoassay, positive cutoff of at least 0.8 U/mL, which tests for the receptor-binding domain of the SARS-CoV-2 spike protein, or the EUROIMMUN enzyme immunoassay, positive cutoff of at least 1.1 arbitrary units, which tests for the S1 domain of SARS-CoV-2 spike protein, both key measures of humoral immune response.4,5 This study was approved by the Johns Hopkins institutional review board; participants provided informed consent electronically.
The proportion of patients who developed a positive antibody response was assessed with an exact binomial confidence interval. The Fisher exact test was used to compare categorical variables, such as antimetabolite immunosuppression, and the Kruskal-Wallis test for continuous variables. All tests were 2-sided with α = .05. Analyses were performed using Stata 16.1/Windows.”
See the full study results, here.
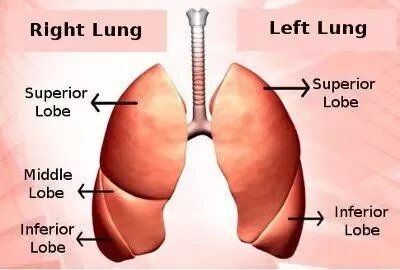
They Survived COVID. Now They Need New Lungs.
“BOSTON — He survived Covid-19, but his lungs were ravaged. After months of deep sedation, he is delirious, his muscles atrophied. And this 61-year-old still cannot breathe on his own.
He was first intubated just after the winter holidays. Now, when he fully wakes, he will see that he is still attached to the ventilator by a tracheostomy tube in his neck. Slowly, he will come to learn that catheters the size of garden hoses are connecting his body to another device, a large extracorporeal membrane oxygenation machine that has taken over the work of his failed lungs.
Gently, his doctors and family will tell him that his lungs are never going to recover, and that this machine is a bridge that will help keep him alive until he can receive a transplant. If it turns out that he is not a transplant candidate — if he cannot build up enough strength, or if he develops a catastrophic new infection or organ failure — the machine will eventually be turned off. And he will die.
He is not alone. Here in my hospital, we are caring for a new population of patients who have cleared the virus but are left with severe lung disease, trapped on ventilators and lung bypass machines.”
Read the full piece, here.
Startup Aims to Make More Kidneys Available for Transplant
“Kidneys are the most in demand organs throughout the country with more than 100,000 people on the transplant waiting list. The tragedy, says a West Lafayette-based startup, is that nearly 30% of the 20,000 kidneys recovered for transplant each year are discarded before they reach the recipient. Renovera, which recently opened space at the Purdue Research Park, is developing technology it says could rescue the vast majority of discarded kidneys and recondition them for transplant. Laser focused on its mission to save thousands of lives, and boosted by Purdue’s aviation might, Renovera says the technology is nearly ready for takeoff.
Renovera founder and Chief Executive Officer Chris Jaynes is confident the startup’s technology could recondition 80% of the kidneys that are deemed unusable, and his word carries weight in the world of transplantation; Jaynes created the technology currently used in the U.S. to rehabilitate donor lungs.
While kidneys are discarded for a variety of reasons, Jaynes says they often hinge on a single element: time. The current U.S. standard requires that kidneys are out of the body no longer than 20 hours to be viable for transplant.”
Full full article, here.
A Patient Pioneer: Minimally Invasive Lung Transplantation
Frank Coburn Is the First Patient in Southern California—and Possibly First in the U.S.—to Undergo the Lifesaving Surgery
“To anyone else, it’s just a walk around the block. But for Frank Coburn, 57, and his wife, it’s a miracle.
A miracle that resulted from Coburn becoming the first Southern Californian—and possibly first in the U.S.—to receive a minimally invasive double lung transplant. The procedure was performed at the Smidt Heart Institute.
“After getting the call that a pair of lungs became available and I needed to be at the hospital immediately, I remember being wheeled into the operating room, finally feeling calm and ready to trust the process,” recalled Coburn, a Huntington Beach resident and longtime boat mechanic. “Once I woke up, my care team shared I had undergone a minimally invasive procedure instead of the traditional, more invasive approach. I was so fortunate and felt so proud to be the first. Truly lucky.”
During a routine lung transplant, surgeons usually create a “clamshell” or sternotomy incision, which involves breaking the breastbone in two pieces and requires many patients to rely on a heart-lung machine.”
Read the full story, here.
Mayo Clinic Q And A: How lung restoration improves organ availability
“DEAR MAYO CLINIC: I was reading about lung restoration and innovation in the field of lung transplantation. Can you share more about this?
ANSWER: Over the past several years, devices outside the body have been used to evaluate human lungs donated for organ transplant before the lungs are transplanted. In the future, lung restoration may increasingly be used to treat donated lungs to make them healthier, so they could be viable for a transplant. The Food and Drug Administration has approved the use of a device known as the Xvivo Perfusion System with Steen Solution Perfusate, which is being used at Mayo Clinic in Florida, in a model constructed to make organs available regionally. Other systems are being investigated.
A lung transplant can be a lifesaving procedure for people with serious lung diseases, such as pulmonary hypertension, emphysema, pulmonary fibrosis, bronchiectasis or cystic fibrosis. But the number of lungs available for transplant consistently falls far short of the number of people waiting for a lung transplant.”
Read the full Q&A, here.
Head of local nonprofit donates kidney to one stranger in order to save the life of another
“WACO, Texas (KWTX) – Coleen Heaton, the director and founder of the nonprofit No Limitations, which was formed to support those in the special needs community through sports and other activities, practiced what she preached about ‘loving with no limitations’ after reading a Facebook post from a friend whose husband needed a kidney transplant.
“I saw a post on Facebook that someone I knew loved someone who needed a kidney. Without much thought or consideration, I looked at my husband and said, ‘What would you say if I said I wanted to donate a kidney?’ And he, knowing me as well as he does and supporting me as strongly as he does, said ‘I guess you’re going to walk around with one kidney for the rest of your life.’”
Heaton had never met her friend’s husband, but after she saw the post on Dec. 16, she contacted the transplant center that night to start the process of filling out questionnaires and testing.
She wasn’t a match for her friend’s husband, but she was a match for another person in need of a kidney and she was told if she agreed to donate to that person, her friend’s husband would also get a kidney in what’s called a paired exchange.”
Read the full story, here.
First COVID-19 Vaccine Dose Elicits Weak Antibody Response in Most KTRs
“Most adult kidney transplant recipients (KTRs) exhibit a weak antibody response to the first injection of the Moderna mRNA COVID-19 vaccine, according to the findings of a prospective study published in Kidney International.1
“We already know that kidney transplant recipients tend to respond less well to vaccines because of the immunosuppression, but data concerning the anti-SARS-CoV-2 antibody response after COVID-19 vaccine in this population were lacking,” said first author Ilies Benotmane, MD, of Strasbourg University Hospital and the Fédération de Médecine Translationnelle (FMTS) in Strasbourg, France.
COVID-19 vaccine distribution programs worldwide have given priority to immunocompromised patients, including KTRs. Vaccination was recommended, however, for this patient population even though KTRs were not included in the vaccine clinical trials. Dr Benotmane and colleagues conducted a preliminary study investigating the efficacy and safety of the Moderna mRNA-1273 vaccine in KTRs by looking at the anti SARS CoV-2 antibody response after the first injection.”
Read more, here.