“My cell phone rang on a Sunday afternoon in early March and I answered it immediately. It was my friend, a doctor who specializes in epidemiology and infectious diseases. She warned me that the coronavirus was about to surge in New York City and recommended that if I could flee the city and retreat to my parents’ house, I should do it, and fast.
I hung up the phone, called my parents, rented a car, packed my bags and drove 13 hours from New York City to the suburbs of Chicago the next morning. Meanwhile, my friends were still going out to dinner and going into work. I could tell my coworkers and roommate thought I was being absurd, but I couldn’t afford to care about their opinions. I had simply fought too hard for all 27 years of my life, I couldn’t lose it here.”
Read the full piece, here.
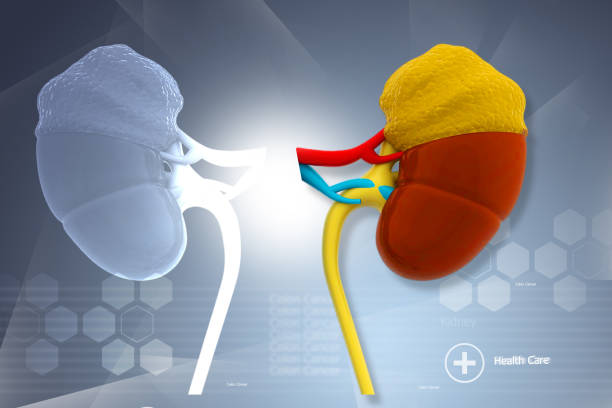
Study examines social determinants of disparities in kidney transplantation
“Among US adults with kidney failure, race and social determinants of health were associated with patients’ likelihood of receiving a kidney transplant. The findings come from an analysis that will appear in an upcoming issue of CJASN.
Blacks are more likely than whites to develop kidney failure, but they’re less likely to undergo kidney transplantation, the optimal treatment for kidney failure. Blacks also have disproportionately lower rates of kidney transplants from living donors, which offer superior patient and transplant survival rates compared with deceased-donor kidney transplants.”
Read the full article, here.
COVID-19 after kidney transplantation: Early outcome and renal function following antiviral treatment
Highlights
- During COVID-19, organ transplant recipients develop all forms of the disease
- This Romanian centre has higher prevalence but similar outcome with other European centres
- Mild and moderate COVID-19 has excellent patient and graft short-term outcome
- Targeted antiviral therapies do not seem to impair kidney graft function
Download the full paper, here.
Tonix Pharmaceuticals and Massachusetts General Hospital (MGH) Enter into Research Collaboration on Tonix’s Third Generation anti-CD40-Ligand Monoclonal Antibody, TNX-1500, for the Treatment and Prevention of Kidney Transplant Rejection
“Transplantation experts led by Tatsuo Kawai, M.D., Ph.D., Surgical Director of the Living Donor Transplantation and Dialysis Access Program at MGH and Professor of Surgery at Harvard Medical School (HMS) will study TNX-1500 in kidney transplantation in a variety of models including non-human primates. The goal of the collaboration is to advance TNX-1500 as a potential first-in-class therapeutic to prevent and treat kidney transplant rejection.
Dr. Kawai said, “Anti-CD40-ligand therapy has a unique activity in controlling the immune response to organ transplants.2 There remains a significant need for new treatments to reduce the toxicity of current treatments by more selectively suppressing immune responses or inducing specific tolerance to the transplanted organ. Anti-CD40-ligand has shown promise not only to effectively suppress rejection but also to facilitate ‘transplant tolerance’ in multiple preclinical transplant models.6”
Read full article, here.
Challenges Facing Transplant Patients in COVID-19 Era
“Transplant patients have an increased risk of developing severe illness when infected with the novel coronavirus. Reports indicate a mortality rate of up to 28% among solid organ transplant patients hospitalized with coronavirus disease 2019 (COVID-19).1
Among the challenges that transplant recipients face is the drug-drug interactions associated with COVID-19 treatment and concomitant medications. For example, remdesivir increases the level of transaminase, which requires close monitoring of liver markers with transplant patients.1
Another challenge is the lack of a test that is sensitive enough to detect active COVID-19-infected donors prior to transplant. Therefore, it’s important to counsel solid organ donors to avoid crowds and monitor exposure for 14 days prior to transplant, whereas hematopoietic cell donors should avoid the crowd for 28 days prior to the scheduled transplant.1“
Read full article, here.
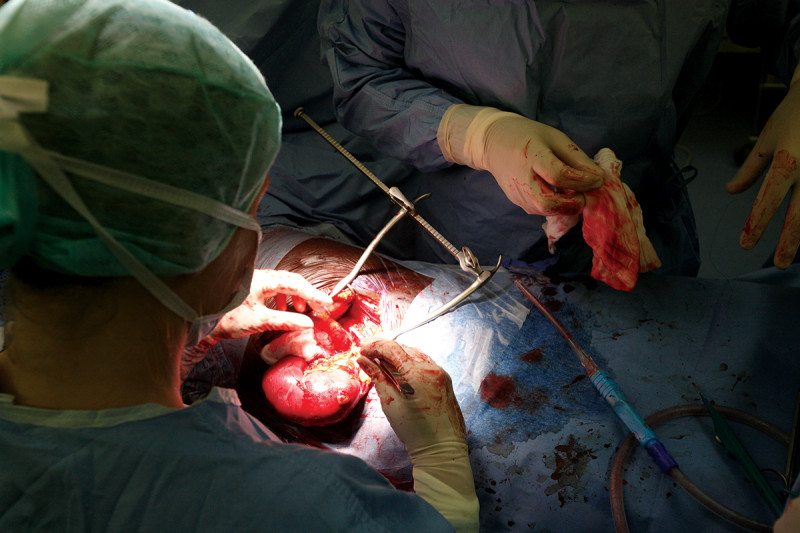
First-of-its-kind Transplant Surgery Saves 11-year-old
“Two years ago, a 9-year-old Baltimore gymnast named Khloe Cox was rising through the competitive ranks, winning awards and following in the footsteps of her hero: Olympic gold medalist Simone Biles.
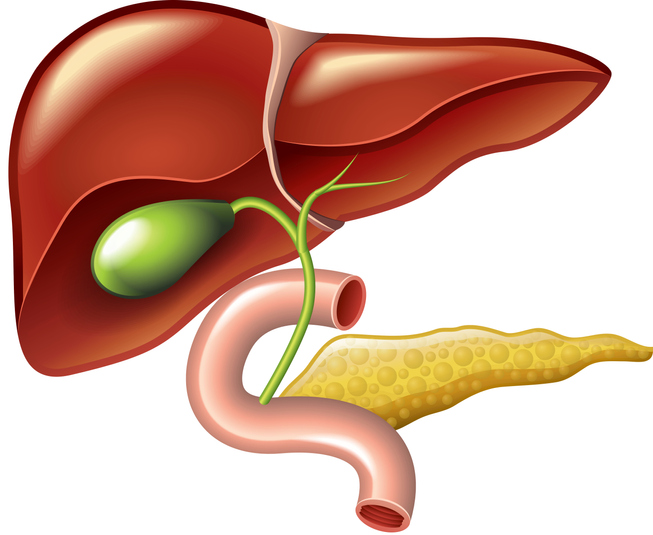
But all that changed one day in 2018, when her parents got a call from her coach. Khloe had fallen ill with a fever and abdominal pain. The young athlete turned out to have a rare stage IV neuroendocrine tumor that had started in her pancreas and spread to her liver.
Khloe needed a dual liver-pancreas transplant, but given her age and the complexity of the surgery, only a handful of surgeons in the world could perform it. Among them was Srinath Chinnakotla, clinical director of pediatric transplantation at M Health Fairview University of Minnesota Masonic Children’s Hospital.”
Read the full story, here.
Kentuckians Need Congress to Approve Lifesaving Bill for Kidney Transplant Recipients
“The COVID-19 public health emergency has revealed painful weaknesses, inefficiencies and inequalities in our health care system. As a result, the public is looking to elected leaders to enact policies that improve our health system, protect at-risk populations and allocate government resources more wisely. Fortunately, there is a bipartisan, common-sense proposal in Congress that could achieve all of those goals for a particularly vulnerable part of the American population: kidney transplant recipients.”
Read the full article, here.
New-Onset Gout as an Independent Risk Factor for Returning to Dialysis After Kidney Transplantation
“Background: The causal relationship between gout and renal transplant outcomes is difficult to assess due to multiple interacting covariates. This study sought to estimate the independent effect of new-onset gout on renal transplant outcomes using a methodology that accounted for these interactions.”
Read more, here.
10 Patients, 5 Kidneys, 1 Story That Will Restore Your Faith in Humanity
“More than 100,000 people are waiting on the kidney transplant list, with some waiting for weeks, months, or even years for the call that could change their life.
That makes what happened at Houston Methodist in October even more extraordinary.
Ten people, including a husband and wife, a boss and her employee, a mother and son, two sisters, and two cousins, took part in a kidney swap. The five pairs were strangers before they walked into the hospital and left with a life-long bond.
Tara and John “HB” Berliski from Magnolia, Texas, have been married for 15 years.
HB started experiencing pain 20 years ago and thought he pulled a muscle. Doctors soon discovered his kidneys were enlarged because of polycystic kidney disease. HB had both kidneys removed, went on dialysis, and waited for a donor.”
Read the full news story, here.
It’s time for Congress to keep its promise to kidney transplant patients
“In 1972, as millions of Americans living with end-stage renal disease (ESRD) struggled to access care, Congress made a commitment to cover the rising costs of their treatment, including kidney transplant. Unfortunately, almost 50 years later, this commitment remains unfulfilled.
Kidney transplant patients must remain on immunosuppressive therapy for life or risk losing their transplant. For nearly two decades, the kidney, transplantation, and donation communities have been advocating to extend immunosuppressive medication coverage for kidney transplant patients beyond Medicare’s current three-year limit.”
Read the full article in POLITICO, here.
To take action and help Finish The Fight, contact your members of congress, here.