Loading
Prior to November of 2020, if approached with the term ECMO or the words ventilator, tracheostomy, or lung transplant, I would have had a grossly rudimentary knowledge of most. Fast forward to January 2021, this would dramatically change as I would have an intimate understanding of what these were. In retrospect, this understanding comes with a high degree of respect for these tools and the people who use them to keep people alive. And that is exactly what they did for me.
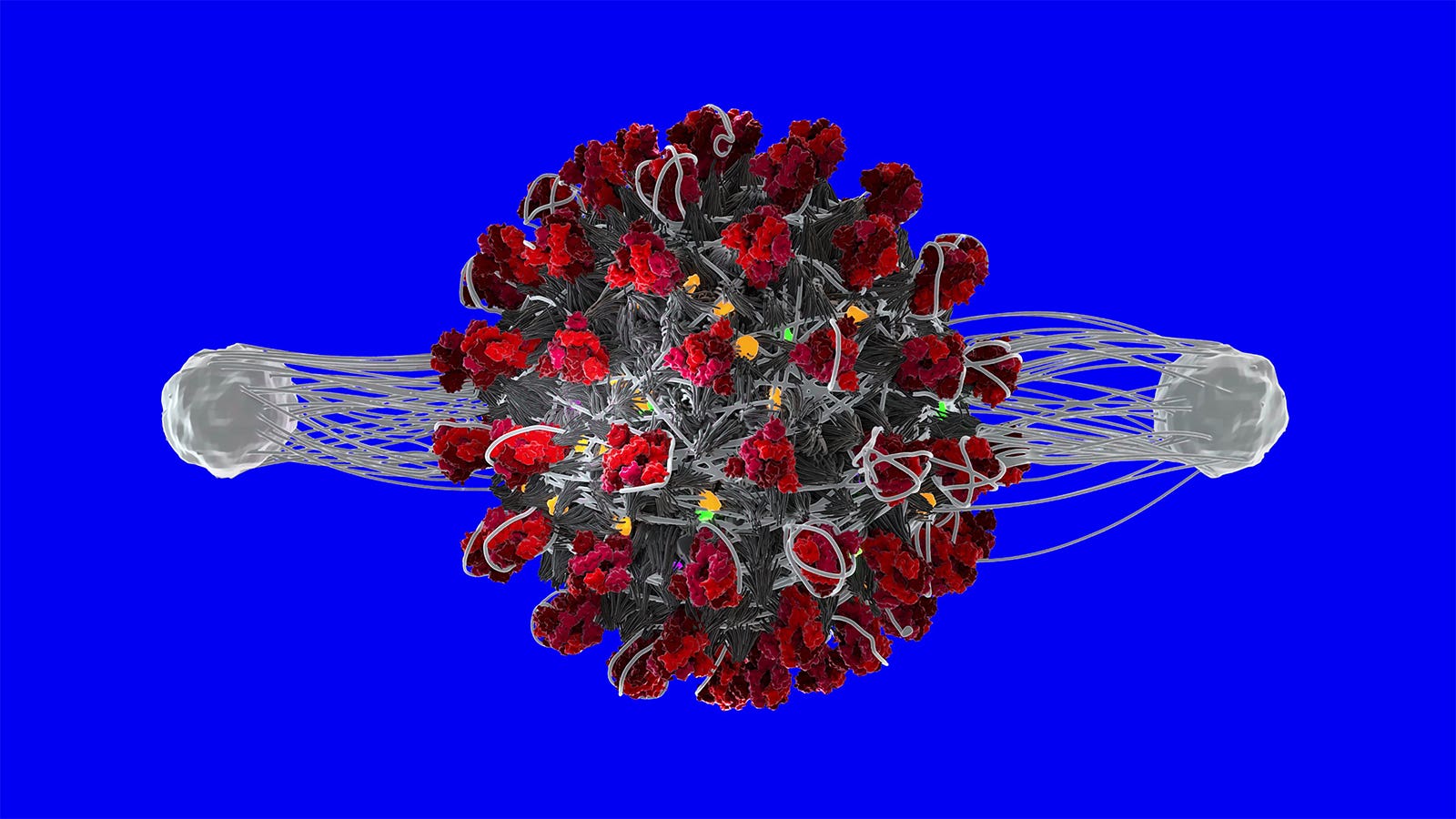
In November of 2020, I contracted SARS-CoV-2, which resulted in my developing Covid-19. The disease ran unapologetically through my body. I had all the classic systems: sore throat, fever, body aches as I have never experienced and horrible fatigue. Realizing I was dealing with something worse than a common cold, I went to my primary care physician for a Covid test. I was instructed to isolate and rest as I waited for the results. After a day of having all these symptoms, I knew this test was going to be positive; and it was.
Read the full editorial in Wiley Online Library.
Loading