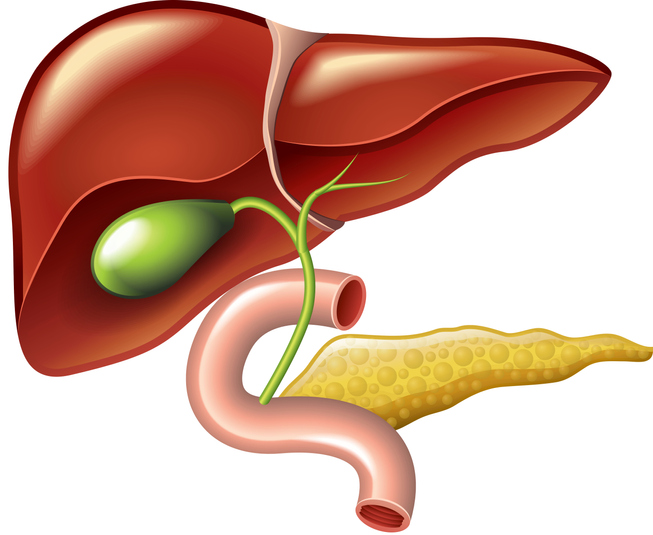
“The liver has many functions that are necessary for life. The liver helps process carbohydrates, fats and proteins, and stores vitamins. It processes nutrients absorbed from food in the intestines and turns them into materials that the body needs for life.
For example, the liver makes the factors that the blood needs for clotting. It also secretes bile to help digest fats, and breaks down toxic substances in the blood such as drugs and alcohol. The liver is also responsible for the metabolism of most drugs.”
Learn more from UNOS here.