By WDTV News Staff
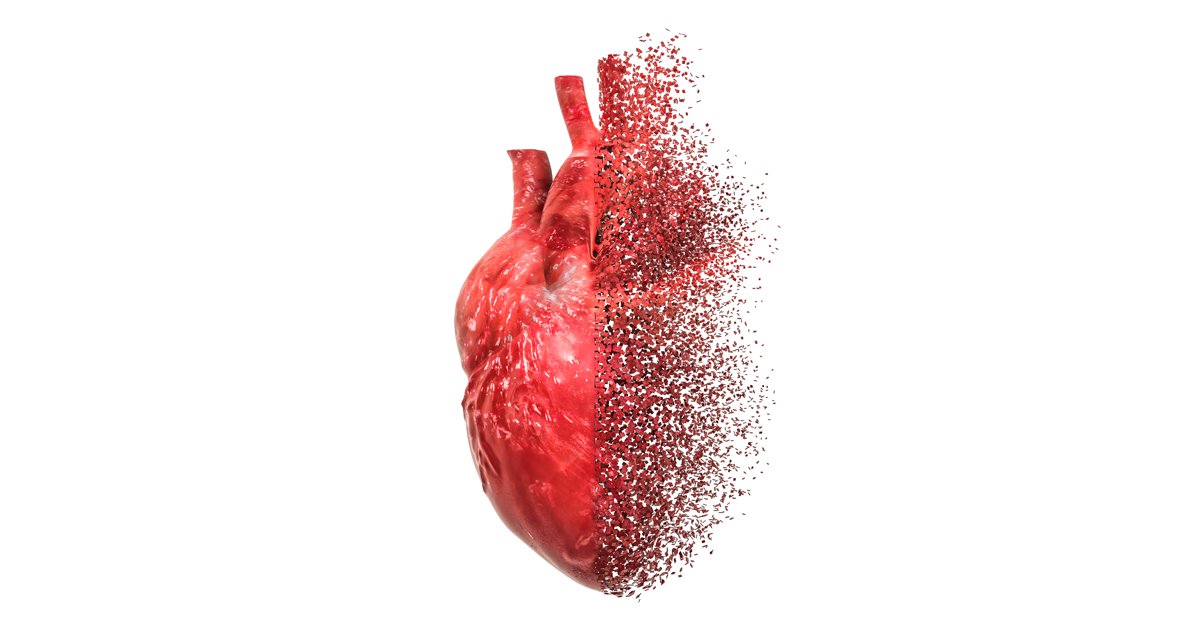
BRIDGEPORT, W.Va (WDTV) – Pediatric heart transplant is a highly specialized form of health care performed at UPMC Children’s Hospital of Pittsburgh. Jasmin Adous tells us more in this month’s Bridging the Great Health Divide sponsored by UPMC Children’s Hospital of Pittsburgh.
The pediatric heart transplant program at UPMC Children’s Hospital of Pittsburgh was the second of it’s kind in the world. Surgeons have performed almost 400 pediatric and young adult heart transplants since 1982. Dr. Brian Feingold is the program’s Director of Heart Failure and Heart Transplantation. He says the program’s success it due to it’s people.
Read the full story from WDTV here.