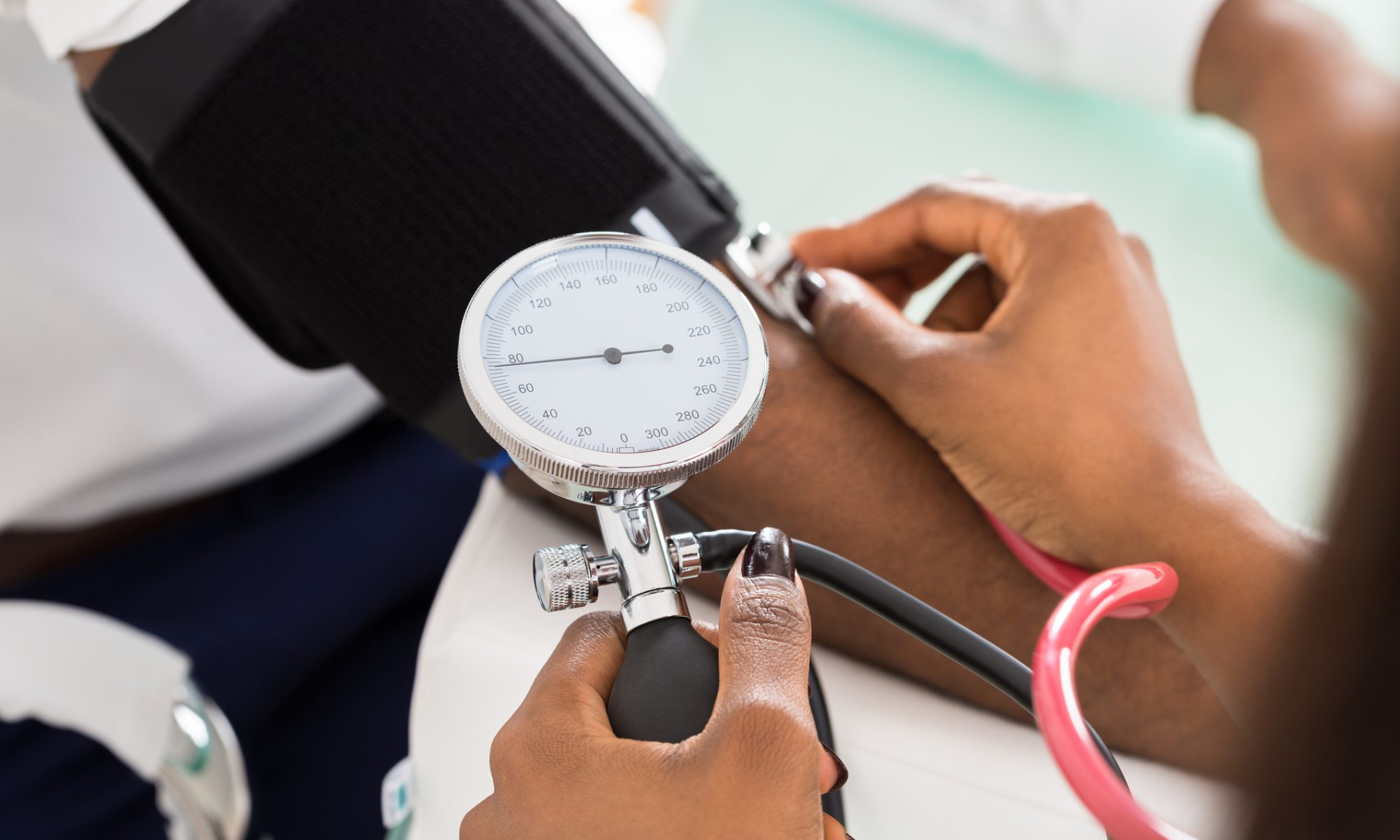
Social determinants of health independently impact post-heart transplant outcomes among Black children.
Social determinants of health (SDOH) independently impact post-heart transplant outcomes among Black children, but not White children, according to the results of a study presented at the American Heart Association (AHA) Scientific Sessions 2022, held from November 5th through 7th, in Chicago, Illinois. Read more from Infectious Disease Advisor.