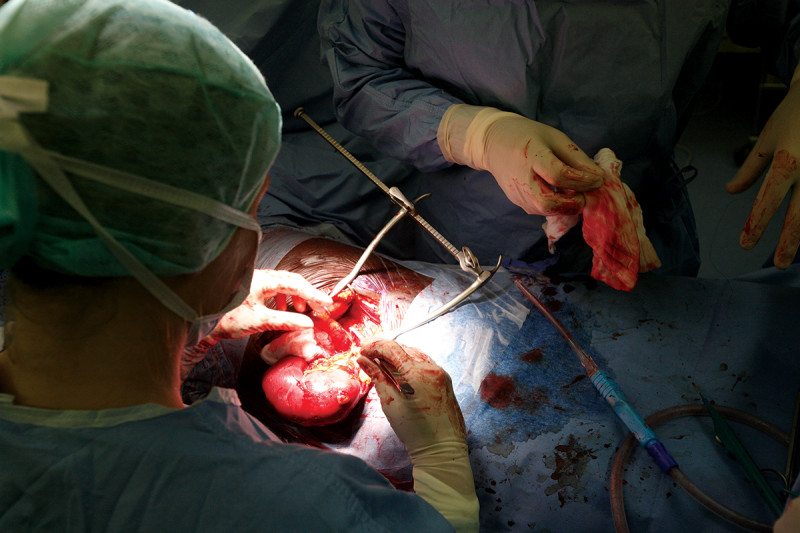
Huntington Beach man has had a second chance at life after he received the nation’s first ever minimally invasive double-lung transplant. 57-year-old Frank Coburn was beginning his second chapter, enjoying life with his loving bride of more than 30 years, and the success of his two adult daughters, when the avid biker started experiencing shortness of breath.
“I would always cough on an intake, and I’d have to kind of belly breathe,” Coburn told CBS2 News This Morning’s DeMarco Morgan.
In March of 2020, he was diagnosed with pulmonary fibrosis.
Read the full story, here.