Loading
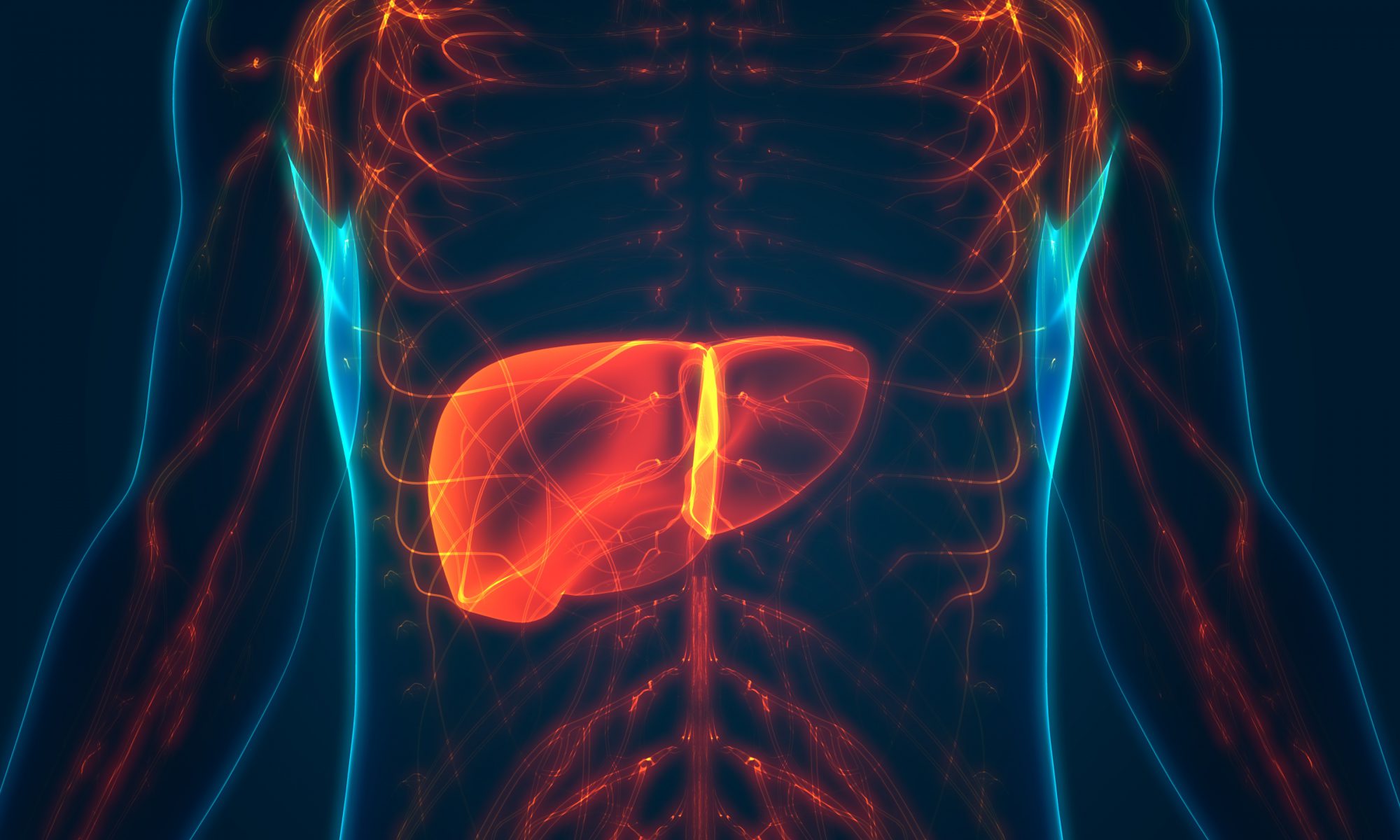
“Outcomes have improved significantly among HIV/Hepatitis C virus-coinfected liver transplant recipients in the direct-acting antiviral era, according to data presented at the Digestive Disease Week.
“The practice of liver transplant for HIV-positive patients has been increasing since 2013 when the HOPE Act was passed; however, the number is still low, less than 1% of total liver transplants,” Jennifer Wang, from the University of Chicago, said during her presentation. “There is a significant geographic variation of HIV/HCV coinfected liver transplant practice with limited number of participating centers. Liver transplant outcomes for coinfected patients have improved significantly in the [direct-acting antiviral (DAA)] era and are comparable to patients without either infection.”
Wang and colleagues analyzed data from the Organ Procurement and Transplantation Network (OPTN) on adult patients in the United States who underwent liver transplantation between 2008 and 2019. They identified 70,125 liver transplant patients, 416 of whom were HIV-infected.”
Learn more, here.
Loading