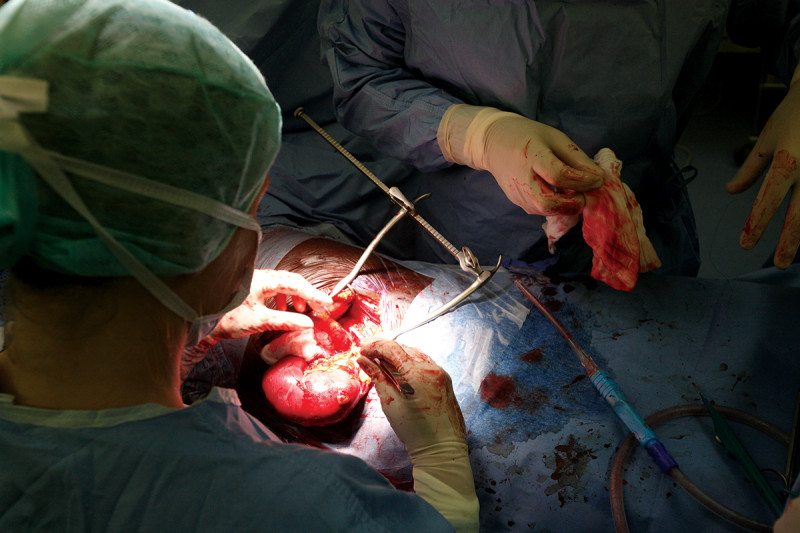
“Patients aged 65 years or older on a waiting list for a kidney transplant may be better off waiting for a kidney from a standard criteria donor (SCD) than accepting one from an expanded criteria donor (ECD), according to recent study.
“The acceptance of an ECD transplant should be carefully balanced against the risks of continued dialysis while waiting for a better donor offer,” investigators Rachel Hellemans, MD, of Antwerp University Hospital in Edegem, Belgium, and colleagues wrote in Nephrology Dialysis Transplantation.
The study included 3808 adult Belgian patients, of whom 3382 received a kidney transplant and 426 were waitlisted and remained on dialysis. The investigators divided patients into 3 age groups: 22 to 44 (1006 patients), 45 to 64 (2213 patients), and 65 years or older (589 patients). The median waiting time on the active waiting list for transplantation while on dialysis was longest for patients aged 22 to 44 years (22.4 months, followed by 18 months for those aged 45 to 64 years, and 11.7 months for those aged 65 years or older.”
Read the full article, here.